Imagine you’re 90 years old, a grandmother of three and your husband is also elderly and ailing. You need help with almost everything, getting out of a chair, going to the bathroom, getting dressed, eating and remembering your medications. Despite advances in life expectancy, ageing has not been kind, and you feel like a burden to your husband and the healthcare professionals who care for you.
Now, imagine being offered a robot that could help with many of these things – from walking to the bathroom to keeping track of your doctor’s appointments. This robot’s advanced artificial intelligence (AI) learns your preferences, knows your birthday and remembers your name. It sounds wonderful, right? You’d no longer feel like a burden to your spouse or depend on carers to help you shower.
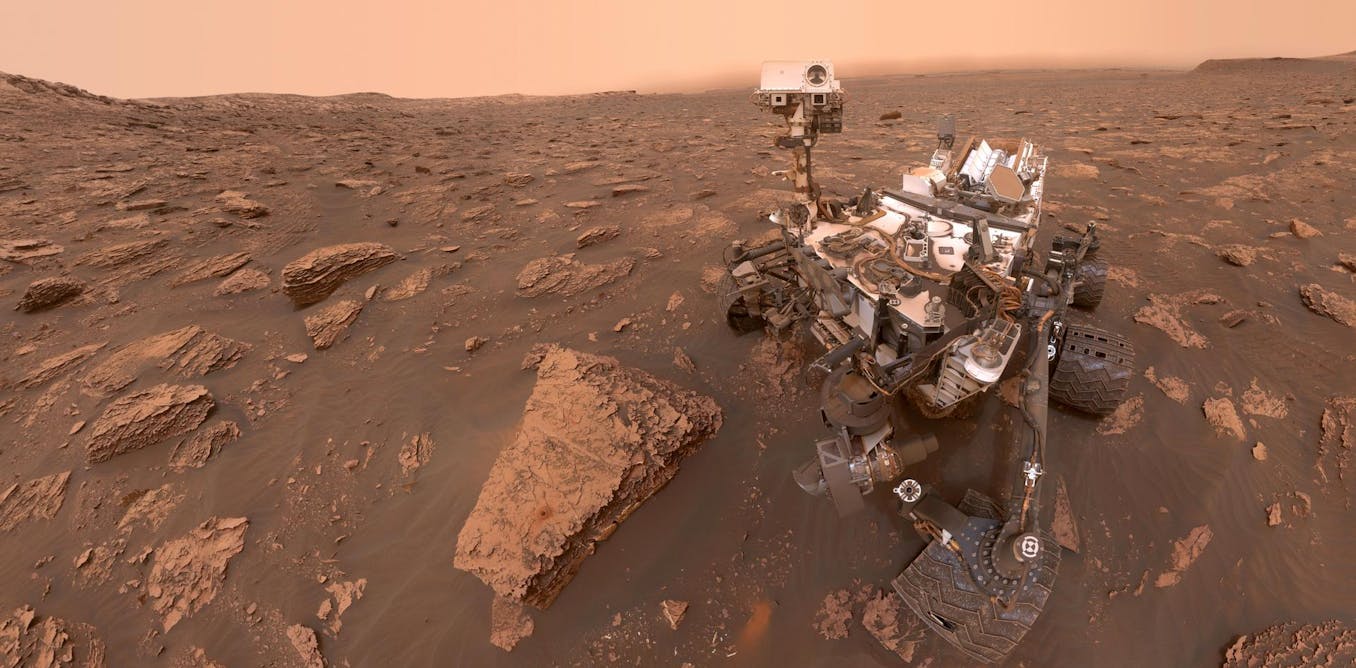
This scenario might seem like the start of a sci-fi movie, but it’s closer to reality than you might think. In Japan, as early as 2018, a survey revealed that older adults living at home would prefer a robot carer over humans.
Japan’s “super-ageing” society, where the proportion of older people is growing faster than anywhere else in the world, has put immense pressure on the workforce. Advances in technology are stepping in to address these challenges, but also present issues for the world’s largest health profession: nurses.
Perhaps understandably, the idea of robot nurses raises concerns in a profession built on the concept of “care” that is often associated with human connections.
A recent study from Australia indicated that giving nursing students awareness of the capabilities of technology generated anxiety and concerns about care becoming less personal. The authors suggested that nurses need to be prepared to “redefine their nursing identity” and called for a “paradigm shift of what nursing is in a digital world”.
These tensions were also apparent in April 2024, when hundreds of US nurses protested against the use of AI in hospitals. The protesters argued that AI tools are untested, unregulated and degrade the value of nursing practice.
One nurse said that “no nurse should be replaced by a robot”, a sentiment that highlights a fundamental issue in healthcare today: nurses are uncertain about their role in a digital world.
This uncertainty seems to have led some nurses to reject technologies – AI-based tools and robotics – that can improve patients’ lives. The key question highlighted by these tensions is, what does it mean to “care” in the digital age?
A universally agreed concept of care may be hard to define, but people using the term often focus on the humanistic and emotional components of caring. In the influential book on nursing, Nursing as Caring: A Model for Transforming Practice (1993), care is defined as: “An essential feature and expression of being human. The belief that all persons, by virtue of their humanness, are caring.”
This definition seems to rule out “care” delivered via new technology, such as robots, as truly caring. But most people would probably agree that denying people access to chemical technologies, such as life-saving medicines, would be considered unjustified and “uncaring”.
The capabilities of new digital technology, like robotics, which may perform roles traditionally undertaken by human nurses, appear to be generating a different response from nurses. This may be because of earlier understandings of care as distinctly human-focused, and because the work robots may provide, such as providing social support to the elderly, is considered “human nature”.
While robots and AI seem to be effective in Japan, the global nursing profession may need to reconsider technology’s role in healthcare. As people live longer and become more dependent on healthcare professionals, the shrinking proportion of working-age people in many developed countries is struggling to meet care demands. Digital technologies could help alleviate this challenge, but the resistance to robotics and AI in nursing is further compounding the issue of overstretched healthcare services.
Historically, though, the healthcare sector has always been slow to adopt new technology. For example, in the UK, the health secretary had to ban the use of fax machines in 2018—19, years after the advent of email. The deadline to phase out fax machines by 2020 was also missed, with hundreds still in use as late as 2022.
In the case of robots, a similar reluctance might not be acceptable to the growing number of people who could benefit from these technologies, particularly as the quality and capabilities of these technologies continue to increase. The future of nursing lies in integrating human compassion with robotic efficiency, ensuring that everyone receives the care they need.
Florence Nightingale, arguably the founder of modern nursing, in her book Notes on Nursing, described her vision of the essence of nursing care. Vague as it was, one thing was clear within this vision, that nurses must focus on the needs of the patient first and foremost and should set aside all other concerns.
I do say that these women had the true nurse-calling – the good of their sick first, and second only the consideration what it was their ‘place’ to do – and that women who wait for the housemaid to do this, or for the charwoman to do that, when their patients are suffering, have not the making of a nurse in them.
That was 164 years ago.
As we stand on the brink of a new era in healthcare, one defined by highly capable machines, it’s crucial that the nursing profession does not let a crisis of professional identity or confused conceptions of care hinder technological advancement.
Nightingale suggests we must not wait while our patients suffer. Embracing innovation while maintaining nursing’s core value – putting the patient’s needs first – can ensure that her vision continues to evolve, meeting the needs of today’s and tomorrow’s patients.

The post “redefining nursing for the 21st century” by Matthew Wynn, Lecturer in Digital Health and Society, School of Health & Society, University of Salford was published on 07/17/2024 by theconversation.com